Advice from Hertfordshire County Council
Wait to be contacted
The NHS will let you know when it’s your turn to have the vaccine. It’s important not to contact the NHS for the vaccination before then.
How you can help
Hertfordshire people have an important part to play to help with the vaccine rollout:
- please don’t contact the NHS to seek a vaccine, they will contact you:
- when they do contact you, please attend your booked appointments:
- please continue to follow all the guidance to control the virus and save lives.
The vaccine is our best defence against the virus alongside effective social distancing, wearing a mask and washing our hands.
The recent rise in cases and emergence of a new variant of the virus also shows that we cannot let our guard down now
You can download the full 15-page COVID vaccines Q&A (dated 31 December 2020) from Hertfordshire County Council’s Director of Public Health Prof Jim McManus.
Below is a summary of the biggest questions many people have.
Key Information Sources
- NHS Information for people receiving the vaccine
- Government Information on priorities for the vaccine
- Patient Information leaflet on the PfizerBionTech Vaccine
- Patient information leaflet on the Astra Zeneca Vaccine
- The COVID chapter of the Green Book
Who is leading the COVID-19 vaccination programme?
NHS England, and locally the NHS Clinical Commissioning Groups are leading patient call ups, policy and deployment. There is nothing local authorities or the Director of Public Health can do on this.
Why am I hearing about only one dose being given now?
Government initially prioritised two doses of vaccine per person with the first priority being those most at risk of death.
There has been a shift away from the discussion around comparing the absolute vaccine efficacy figures – towards just focusing on reducing the severity of COVID-19 illness, getting as many people with some immunity as possible and keeping people out of hospital – even with just one dose of the Oxford AstraZeneca vaccine.
This is a sensible and pragmatic decision that has been backed up by scientific advisors and is sensible given where we are in the current surge of infections. Because the vaccine also reduces disease severity if you do get it, a one dose strategy is an option to help reduce the burden on health care.
Can I get the vaccine if I have had COVID-19?
There is no problem with receiving this vaccine after having had COVID-19 already. This is the same for the seasonal flu vaccine.
Is one dose rather than two safe?
Yes. And remember this is only initially. The intention remains to give everyone two. The government has decided, after consulting scientific experts to extend the gap between the first and second doses.
There may be a delay of up to 12 weeks between first and second dose, which is longer than the originally forseen 28 days gap.
The Joint Committee on Vaccination and Immunisation (JCVI) conclusion is that this gap is safe, and will enable initially many more people to be given a single dose of vaccine. The aim of this is to help build population immunity as rapidly as possible
Who can get the COVID-19 vaccine?
The NHS is currently offering the COVID-19 vaccine to people most at risk from coronavirus. The vaccine is being offered in some hospitals and by the end of January there will be hundreds of local vaccination centres run by GPs.Some are already up and running in Hertfordshire
In the next two months it is being given to:
- people aged 80 and over who already have a hospital appointment in the next few weeks
- people who live or work in care homes
- health care workers at high risk
You will also need to be registered with a GP surgery in England. You can register with a GP if you do not have one. The vaccine will be offered more widely, and at other locations, as soon as possible.
The order in which people will be offered the vaccine is based on advice from the Joint Committee on Vaccination and Immunisation (JCVI).
Two Phase Roll Out
The vaccine is being rolled out in two phases. In phase 1 the aim will be direct prevention of mortality and supporting the NHS and social care system
- residents in a care home for older adults and their carers
- all those 80 years of age and over and frontline health and social care workers
- all those 75 years of age and over
- all those 70 years of age and over and clinically extremely vulnerable individuals
- all those 65 years of age and over
- all individuals aged 16 years to 64 years with underlying health conditions which put them at higher risk of serious disease and mortality[
- all those 60 years of age and over
- all those 55 years of age and over
- all those 50 years of age and over
- It is estimated that taken together, these groups represent around 99% of preventable mortality from COVID-19.
The second phase will focus on further reduction in hospitalisation and targeted vaccination of those at high risk of exposure and/or those delivering key public services
As the first phase of the programme is rolled out in the UK, additional data will become available on the safety and effectiveness of COVID-19 vaccines. This data will provide the basis for consideration of vaccination in groups that are at lower risk of mortality from COVID-19.
Phase 1 is the biggest single logistics exercise in the history of the NHS.
Is there anyone who shouldn’t get the vaccine?
There are some people who shouldn’t get the vaccine. People with a history of severe allergies to vaccines, people with very immunocompromised systems (e.g. just after organ transplants) and some others.
It is important to tell your clinician your full medical history. For some people antibody therapy will be made available through their specialist clinical team.
What about people on blood thinning treatment?
Many people on blood thinning treatment can have it under certain conditions. Again tell your clinician about your medication and clinical history
What about people with HIV?
The British HIV Association has issued guidance. People with HIV who have an undetectable viral load and are stable can receive the vaccine.
What about pregnant women?
The JCVI has stressed it does not recommend giving the vaccine to pregnant women or children under the age of 16 because at present we do not have enough information on the effects of vaccination during pregnancy.
This is a normal precaution. Public Health England agrees pregnant women should not be given the vaccine.
What about vaccinating children?
Government says COVID-19 vaccines are not routinely recommended for those under 18 years of age, due to lack of data. That may change.
It is unclear how quickly this means a vaccine will be given to 16-18 year-olds who have underlying health conditions, as per the JCVI’s priority list above.
What about teachers and unpaid carers?
This is a matter for Department of Health and Social Care to decide and local areas cannot influence or change the arrangements, but are lobbying to have unpaid carers and teachers put higher in the priority list.
What about other key workers?
Again this is a matter for Department of Health and Social Care to determine.
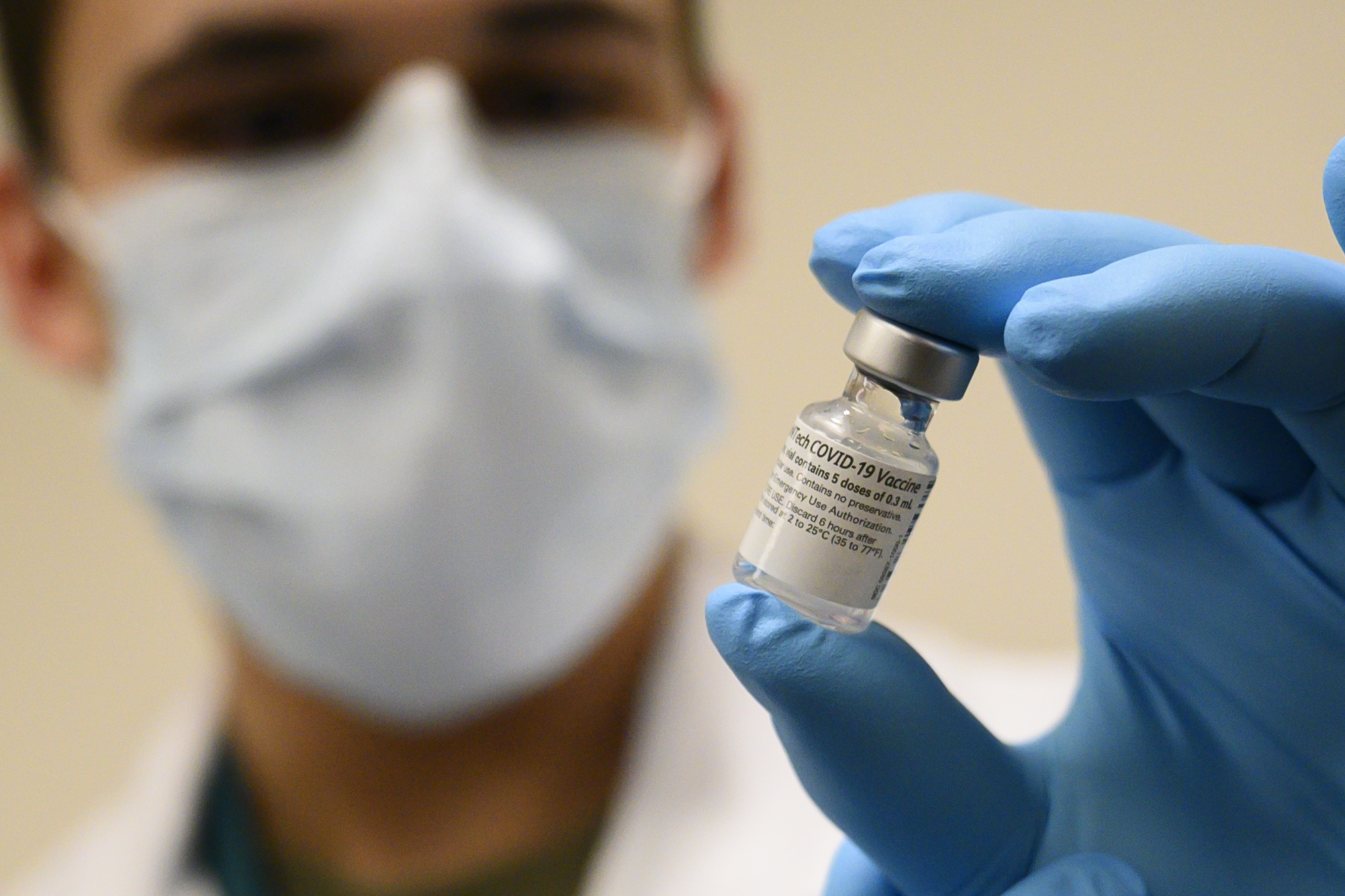
Which vaccines are available?
Two vaccines have been licensed for use in England, the Pfizer-Biontech Vaccine and the Oxford/Astra Zeneca Vaccine. More will be available in due course.
How will people be notified?
Patients will be sent a letter by the national NHS call/recall service telling them they are eligible for vaccination and that they have a choice of where they can get their vaccine.
Meanwhile, Primary Care Networks (groups of GPs) will also be expected to contact patients eligible for vaccination, using nationally agreed wording. Patients will be given the choice to either book at a GP-led vaccination centre or use the national booking service to be vaccinated by another provider.
When will I get called?
You will get called in strict rotation when practices are ready. Not all Primary Care Hubs are going at the same pace for a variety of reasons. But the NHS will call you. If you are NOT registered with a GP then you need to register now in order to be called.
Who will be able to administer the vaccinations?
Registered healthcare professionals will need to carry out the clinical assessment, consent and preparation of the vaccine.
However, the vaccine itself can be administered by a suitably trained non-registered staff member – while under the clinical supervision of a registered healthcare professional.
Will patients need to be monitored after being given the vaccine?
It is standard after vaccines to ask people to wait a few minutes. The same should happen with ‘flu vaccine. You may be asked to wait five or ten minutes to check you don’t have a reaction. This is entirely normal.
Can two different types of COVID vaccine be used with the same patient?
Yes – though Public Health England says every effort should be made to complete both doses with the same vaccine where possible.
That is because there is currently no evidence on the interchangeability of vaccines. But PHE says since both frontrunners are based on the spike protein of the virus, it is likely the second dose will help to boost the response to the first dose even if a different vaccine candidate is used.
How quickly does immunity kick in?
The Pfizer vaccine provides immunity seven days after the second dose is administered. The Commission on Human Medicine (CHM), which advises the Government, says partial immunity does occur after the first dose but two doses guarantees the best immunity.
The Oxford AstraZeneca vaccine immunity builds continuously from 7 days onwards with one does providing 70% effectiveness within 28 days.
The efficacy of two doses is in the range of 80% for the Oxford vaccine and 90% for the Pfizer Vaccine. This is good efficacy for each vaccine.
Are there any side effects of the vaccines?
Side effects such as a sore arm or reaction are normal with vaccines. It shows the body is reacting. The Government has said no serious safety concerns were reported in the trials.
Side effects from both vaccines are caused as part of the immune response to the vaccines. In some ways, the more vigorous the immune response, the more common the side effects.
The most common side effects from the vaccines are:
- Fatigue
- Headache
- Muscle aches
Side effects occurred during the first week after vaccination, but were most likely one or two days after receipt of the vaccine.
Side effects were more frequent following the second dose and more likely to be experienced by younger, rather than older, recipients.
Although most people will not have significant side effects, some people may wish to schedule their vaccination, so that they will not need to call out of work the next day if they don’t feel well
A patient leaflet is given with each vaccine.
How long will protection last and will there be annual vaccinations?
We should know when the various vaccination candidates are approved. As yet we cannot be sure how long the vaccine lasts
Does a vaccinated person present a risk to unvaccinated family members in the same house?
The vaccines are not composed of live viruses, so there is no infectious virus to spread from a vaccinated person to someone else.
But, we do not yet know if a vaccinated person who encounters the virus can still experience what is referred to as “asymptomatic infection”.
An asymptomatic infection occurs when a person is exposed to the virus in the community and the virus can still replicate in their body, but they don’t have symptoms because their immune system stifles the infection as a result of vaccination. In this scenario, the person could potentially spread the virus without even knowing they are infected.
Given that families may not all get vaccinated at the same time, those who have been vaccinated should continue to practice public health measures when they are out in the community to decrease the chance of introducing the virus in the home through asymptomatic infection.
Likewise, even when a whole family is vaccinated, continuing to practice these measures will be important for two reasons:
- The vaccine will not work for everyone, so someone in the home who has been vaccinated may still be susceptible.
- People outside of the family’s “bubble,” like co-workers, extended family members, neighbors, and others they come into contact with, may not have been vaccinated (or may be in the group for whom the vaccine does not work).
This approach will be important until we can get control over the spread of virus. Once enough people have been vaccinated to slow the spread of the virus, we will all be able to move away from these public health measures. But, for now, we need to continue working together to decrease spread of the virus by masking, physical distancing, handwashing, and getting vaccinated.
No responses yet